THE FIGHT TO END MOTHER-TO-CHILD TRANSMISSION OF HIV

The state of play
We know that health systems increasingly have the resources to address mother-to-child transmission (MTCT) of HIV; but, in practice, these resources often go under-utilised.
Encouraging mothers to attend clinic appointments, remain adherent and accept support from their partners, family and broader community are all important factors that will contribute to ending MTCT.
In recent years, there has been significant progress towards this goal. In 2010, 280,000 children were infected with HIV and by 2016 this number had dropped to 160,000.1 However, the global target for 2020 is 20,000 a year.2 There is more work to be done if we are going to meet this target as a global community.
So, where do we start?
Joining the dots: the HIV care continuum
The HIV world often talks about a ‘continuum of care’ – ensuring that people at risk of HIV get tested; that those who are tested receive antiretroviral treatment (ART); and those on ART achieve and maintain viral suppression. This is easier said than done given the prevailing attitudes towards HIV and particularly the stigma and discrimination that exists.
In many resource-limited countries where the prevalence of HIV is high, this continuum is sometimes disjointed; with one end not speaking to the other. For example, in some areas where testing is taking place and making in-roads, very few of those testing positive for HIV are being referred to their local clinic to receive treatment.


There are many challenges that are present in ending the HIV epidemic, and mother-to-child transmission is simply one of them. Only by joining forces and fighting on all fronts can we begin to contain it.
Without a bold and empowered community response, the health system, operating in isolation, will not succeed in breaking down many of the barriers preventing access and retention in HIV care programmes – such as HIV stigma.
It’s clear that in order to reach and retain record numbers of pregnant women, children and adolescents living with HIV in care, clinics and communities must work together. Their combined efforts will ensure there is an increased uptake of care, children and families are linked to HIV support services, stigma and discrimination is combatted, care programme quality is monitored, and stronger local health systems are built.
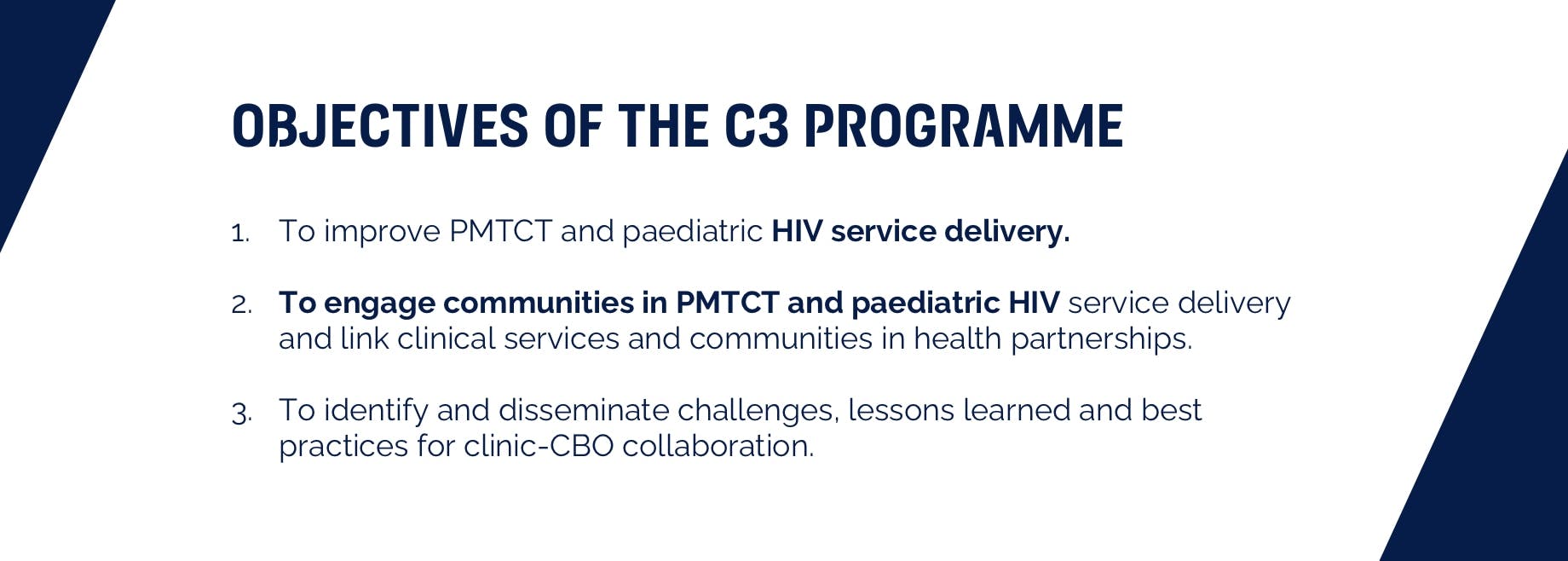
That’s where the Clinic-Community-Collaboration (C3) programme comes in…
The C3 programme, with funding from our Positive Action Programme - which works to ensure that no person living with HIV is left behind - promotes clinic-community collaboration as a key strategy in the elimination of MTCT of HIV.
Through work with the action network, Paediatric & Adolescent Treatment Africa (PATA), partnerships have been fostered between health facilities and communities, enabling them to deliver improved prevention of mother-to-child transmission (PMTCT) and paediatric HIV services together.

Has it worked?
Since its initiation, the programme has worked across nine countries (Cameroon, Democratic Republic of Congo, Ethiopia, Kenya, Malawi, Nigeria, Uganda, Zambia and Zimbabwe) and 36 community-clinic collaborations demonstrating first-hand how transformative collaboration at a local level can be to a health response.
Results from the programme showed important improvements in clinic-community partnership indicators and an increase in women enrolled in PMTCT services with fewer people living with HIV lost to follow-up.
In addition, according to data from all 36 partnerships, C3 showed improved relationships between clinics and community-based organisations (CBOs) and an improved perception of each other’s contribution to PMTCT/ paediatric HIV care services,
ViiV Healthcare: proud to support
We’re proud to say that C3 has played a significant role in creating a growing community of practice centred around clinic-community collaboration and generated rich and diverse insights and learnings that will directly contribute to achieving improved community engagement.
The programme has also led to the development of two toolkits: one focussed on paediatric care; the other on differentiated service delivery for adolescents. Both toolkits drive home the importance of clinics and frontline health workers, working together with the community and community organisations.
There is, however, more to do, which is why we are continuing our support to PATA beyond our initial commitment, through our new strategic Positive Action Breakthrough grants. The scheme makes grants available to projects working towards ending paediatric AIDS in priority areas by 2025.
For more information and resources, including access to the C3 toolkits and online course, please visit our partner PATA’s website at https://teampata.org/c3/
References:
- UNAIDS. Fact sheet. Available at http://www.unaids.org/en/resources/fact-sheet. Last accessed: June 2020.
- Start Free. Stay Free. AIDS Free. A Super-Fast-Track Framework for Ending AIDS in Children, Adolescents and Young Women by 2020. Available at: https://free.unaids.org/. Last accessed: June 2020
YOU MAY ALSO BE INTERESTED IN:
Positive Action Global’s mission is to be a transformational partner that champions people and communities to end AIDS. Our vision is Healthy Communities in a World Free of AIDS.
The Global Positive Action 2020-2030 strategy works towards achieving healthy communities in a world free of AIDS and embodies our mission of leaving no person living with HIV behind.
NP-GBL-HVX-COCO-230010
If you get any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the GSK Reporting Tool link https://gsk.public.reportum.com/. By reporting side effects, you can help provide more information on the safety of this medicine.
If you are from outside the UK, you can report adverse events to GSK/ ViiV by selecting your region and market, here.

