BRIDGING THE HEALTH INEQUALITY GAP IN HIV: THE ROLE OF REAL-WORLD EVIDENCE IN CLINICAL SETTINGS
Health inequalities have existed and persisted for decades. By expanding our knowledge of diseases and how treatments work in real-world settings, we can help close the gap in health outcomes for patients who have been historically underrepresented.
There is no doubt that we need clinical trials in HIV care. Randomised clinical trials (RCTs) are the gold standard for research and the first clinical trials of the 1980s were a cornerstone in the response to the HIV epidemic. But from day one, it was apparent that only certain groups were represented in those trials. Still to this day, white men make up the majority of clinical trial participants, however, HIV can affect anyone regardless of race, age, gender identity, sexuality, or class.1
So why is representation in data needed? In addition to ensuring that we truly understand the safety and efficacy of therapies across all subgroups, representation also means that people are able to see themselves represented in data. In doing this, we can ensure people feel seen, valued, and heard. RWE offers an opportunity to capture the experiences of diverse groups of people which we don’t always see in clinical trials, allowing for improved, more personalised clinical decision-making and ultimately better health outcomes for all patients.
The rise of health literacy: Making RWE accessible
The past four decades saw huge progress made in HIV research, along with the technology used to record, store and access data, meaning that people living with HIV often have greater ability to obtain, understand and use healthcare information – formally known as health literacy. Community organisations and peer supporters have been at the forefront of providing information and improving health literacy across the HIV community. Alongside these important organisations, we must make an intentional effort to ensure different languages, reading levels, and access methods are addressed. As clinicians, our role is to ensure that people can access the right information about, for example, available treatments, latest research, and holistic health support. This can be made easier through technology, such as sharing information with patients via WhatsApp. However, it is important to acknowledge the digital divide affecting some people living with HIV and ensure that online sources are not the only ways to disseminate information to those who need it.
As well as thinking about how we present the data we do have, we also need a level of honesty about the data we don’t have if we want to maintain trust with the people who rely on us for supporting their health. For example, it is clear that we don’t have enough women represented in RCTs, along with varied ethnicities, diversity in age or sexuality, and even different socioeconomic circumstances. If people are unable to feel seen, they may not feel respected, protected or valued, leading to decreased engagement in care and a risk of poor adherence to treatment. We need to be honest about barriers changing the protocol of clinical trial recruitment in addition to making a conscious effort to acknowledge the unique lived experiences of the people we see and factor that into how we share information. All this while working to challenge and address these barriers.
From clinical trial to clinical practice: How clinicians can collect and share RWE
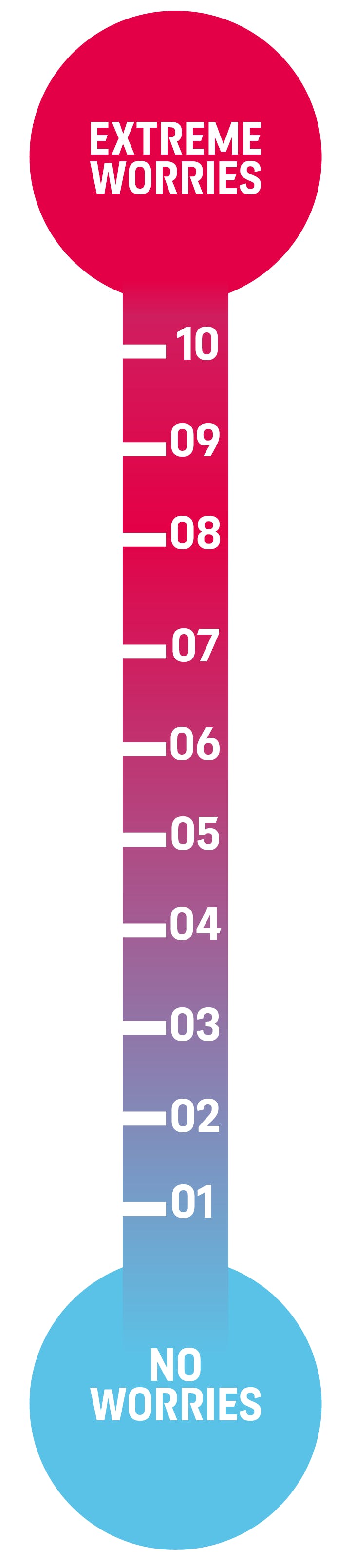
As a HIV clinician, I want my patients to feel comfortable enough to be honest about their experiences so that I can factor it into any treatment decisions in combination with what the data tells me. Being able to understand where someone is in their life at the moment, and how that ultimately influences their decision-making and behaviour, brings a real-world depth to clinical decision-making, allowing for healthcare providers to evaluate whether a particular treatment is truly the right choice for a person living with HIV beyond what prescription guidelines tell us. This does, however, put pressure on us as clinicians to record as comprehensive notes as possible during the time allowed, meaning the most salient points are often recorded and other important aspects may appear lost. This highlights the value of additional opportunities or methods of data collection, for example the ‘distress thermometer’ I implement in my consultations to capture a fuller picture of what my patients are truly experiencing. Collaboration is key to maximise impact from RWE – be it sharing data from your cohorts with colleagues to piece together the picture of how a treatment performs across diverse groups, or working with patients to get the most out of consultations and gain real-world insights on both an individual and a community level.
RWE in the future: UNAIDS and beyond
We have come so far in our efforts to treat HIV, and the fight is not yet over. With each new drug class, administration method, or formulation, the realm of HIV research expands even further. So where does RWE sit in this? It is encouraging to see that awareness of real-world data and its value is increasing, though it is now more important than ever for us to address health inequalities affecting underrepresented populations and capture the social and behavioural determinants of health. One way of achieving this which I am particularly excited about is the appearance of studies with protocols that intentionally recruit a certain percentage of people to represent groups across age, gender, and ethnicity, along with research in commercial settings that consider different populations from the beginning. RWE can take this further by providing another opportunity for in-depth exploration, for example employment characteristics, which paints a fuller picture of the multifaceted lives of people living with HIV. And this shouldn’t stop at clinical settings. Pools of real-world data need to be disseminated globally, allowing for analyses of how efforts against HIV are advancing on local, national and global scale – for example, RWE can give insights into what infrastructure or environmental changes are needed to support progress towards the UNAIDS 95-95-95 targets for 2030, as well as illustrating dynamic changes that might indicate that goals aren’t actually being met when they otherwise seem to be.
If we are to optimise the way we care for people living with HIV and reduce health inequalities, we must leverage real-world evidence to ensure patients benefit equally from the latest care innovations. Taking this a step further, as patients grow more health literate, we must ensure the real-world evidence we are collecting is made accessible. Sharing real-world evidence with our patients can help to build trust and ensure all people living with HIV feel seen.
If you get any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the GSK Reporting Tool link https://gsk.public.reportum.com/. By reporting side effects, you can help provide more information on the safety of this medicine.
If you are from outside the UK, you can report adverse events to GSK/ ViiV by selecting your region and market, here.
