IMPLEMENTATION SCIENCE
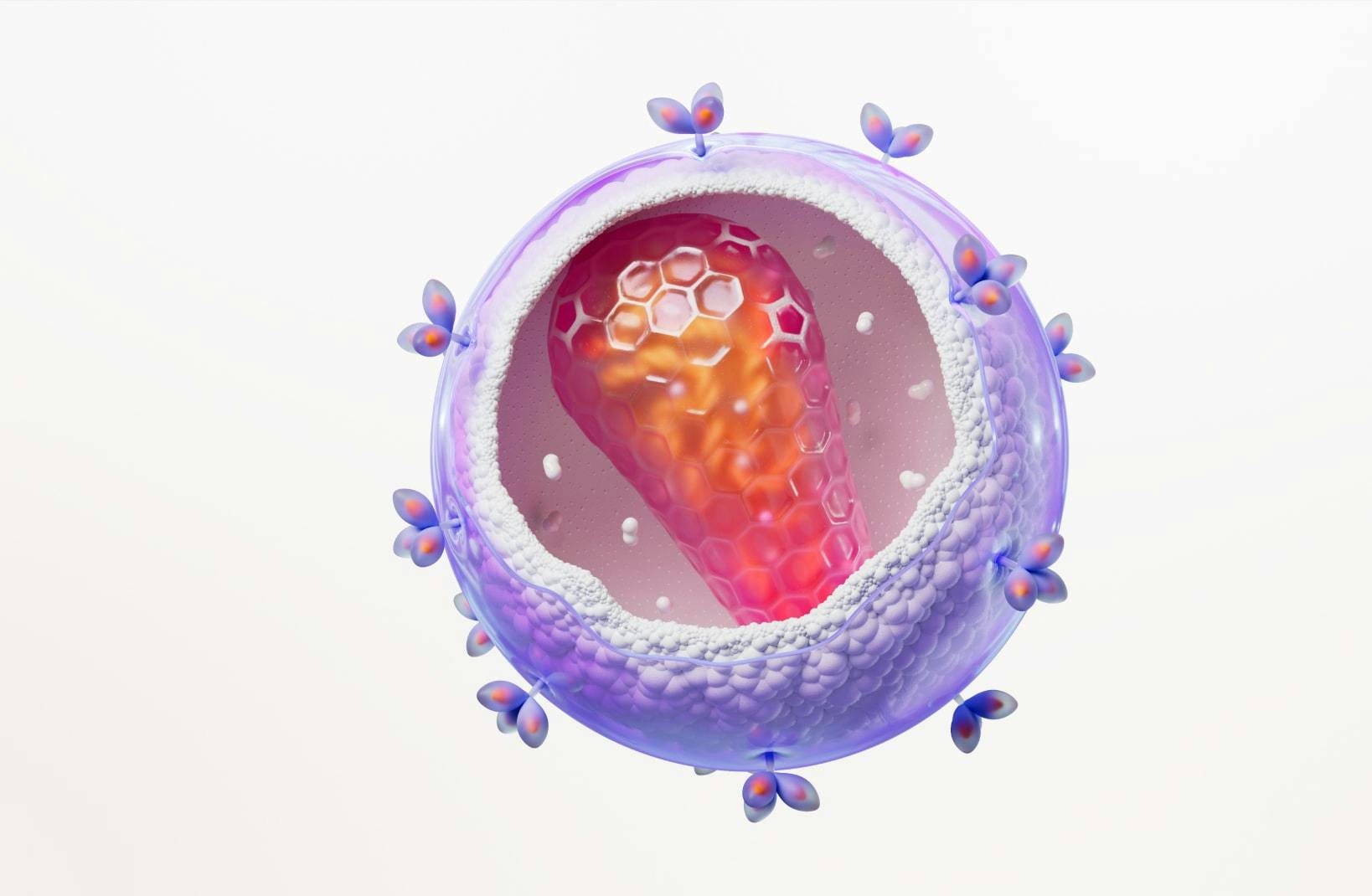
Maximizing the impact of HIV prevention and treatment by bridging the gap between research and clinical practice.
ViiV Healthcare, the only company solely focused on HIV, is leading the way in HIV Implementation Science. We invest in research to bridge the gap between clinical trials and real-world HIV care, aiming to improve testing, diagnosis, retention in care, and community viral load suppression.
Implementation Science is the study of methods to promote the integration of research findings and evidence into healthcare policy and practice. We collaborate with researchers, public health leaders, academia, governments, and community organizations to maximize the impact of implementation research. Our goal is to enhance the lives of those affected by HIV and prevent its spread.
We are dedicated to identifying strategies to bridge the gap between the availability of effective HIV medications and the access and use of those medicines to better the lives of people living with HIV and of people who can benefit from PrEP.
Digital Innovation & Implementation Science
Digital Innovation and Implementation Science leverages research and digital solutions to transform HIV care, prevention, and experiences. Striving to lead the industry, our solutions include developing support tools, educational materials, diagnostic innovations, and wearable technology, all with the goal of improving experiences for patients and providers.

NP-GBL-HVU-WCNT-250001 | January 2025
If you get any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the GSK Reporting Tool link https://gsk.public.reportum.com/. By reporting side effects, you can help provide more information on the safety of this medicine.
If you are from outside the UK, you can report adverse events to GSK/ ViiV by selecting your region and market, here.